After our successful oocyte (egg) retrieval and semen collection we can finally start the next stage of IVF - the fertilisation!
The whole fertilisation process that happens in the embryologist’s lab is incredibly fascinating to me. First of all, the embryologist has to find the oocytes in the follicular fluid, which was collected from the follicles during the oocyte retrieval. The doctor has only a few minutes for this process because the oocytes do not tolerate the change of their environment well. The oocytes, are then transferred to an incubator, which provides the perfect conditions for growth - the incubator simulates the womb. At the same time, the oocytes are cleaned from other cells to make sure that there aren’t any disrupting elements during the fertilisation of the oocyte.
By the end of the procedure, we had three mature oocytes ready to be fertilised. In our case, two out of our three fertilised oocytes were developing properly in the laboratory. We have to understand that nature also plays a role in this process, even though it is happening in a controlled environment. If there is a genetic problem with the oocyte or the sperm, nature intervenes, which, in my opinion, is the way it is supposed to be
On day three after the oocyte retrieval, the doctor let us know the great news: we had two beautiful, well-developed embryos that were patiently waiting and looking forward to returning to their mother's uterus.
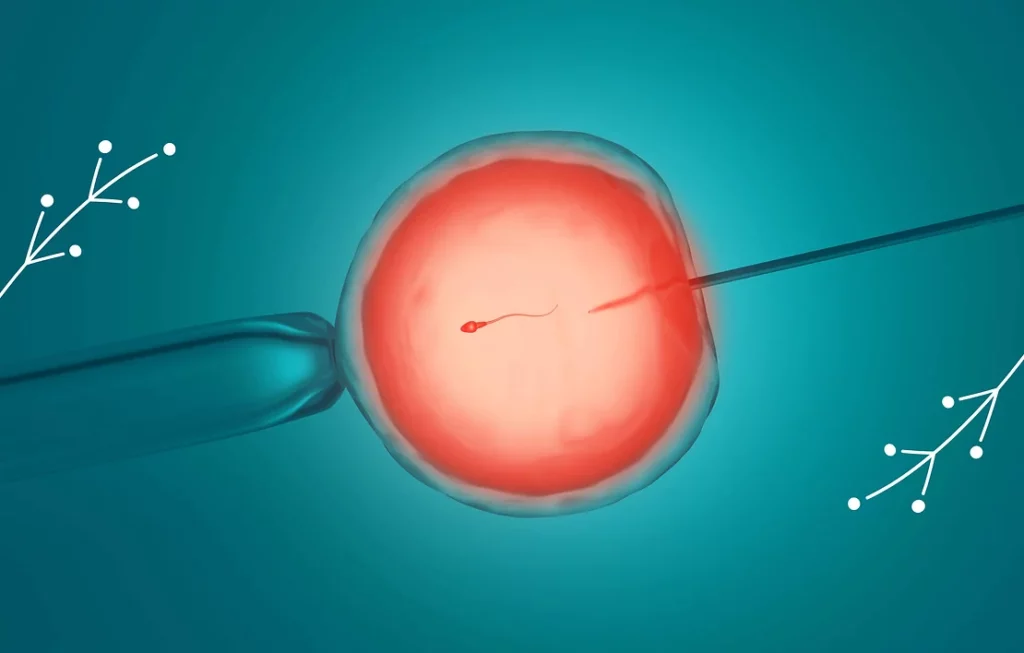
A similar procedure must be applied to the semen as well. The process of filtration chooses semen with the best motility (movement) and morphology (shape). After careful selection, the semen are washed from residual seminal fluids. Following the preparations, the embryologist selected the three finest sperms from the remaining sample. Each of these three sperms were injected into one of our three oocytes. This is a simplified version of how fertilisation is done.
The direct injection of sperm into an oocyte is called ICSI, or intracytoplasmic sperm injection. This protocol is mainly used when the sperm count, shape or movement are deteriorated and the sperms need a little help from the embryologist to increase the chances of fertilisation. Personally, I would have preferred to do this process the way nature intended to, meaning, let the thousands of sperm swim towards the oocyte in the culture dish and let the strongest one achieve the goal of fertilisation. Nevertheless, in our case doctors recommended ICSI as the method with the highest probability of success.
After fertilisation the oocytes are moved back into the incubator, which provides an optimal environment for their development. If everything goes according to plan, the fertilised oocytes will begin to divide. After the first 20 hours they undergo a thorough screening process during which the embryologist examines the oocytes to check for signs of fertilisation. Later, about 48 hours after ICSI, the oocytes are checked again. It takes up to 5 days until the embryologist can tell for sure if and which oocytes are fertilised.
The emotional numbers game of counting follicles, oocytes, hopes, and dreams.
Today is day 1 after my oocyte (egg) retrieval (known simply as OCR in the IVF community). The phone call with my fertility clinic is scheduled for 9am to receive some details about yesterday's events. At 9am I dial the number that I found on the document that I received after my oocyte collection. I turn on the speaker on my phone to make sure that my husband does not miss any information. A very kind voice answers the call and the woman introduces herself as our embryologist. After a short identification process, she informs us that she found two mature oocytes out of the five that were collected yesterday, and one of the two was successfully fertilised.

I am speechless. That is not the news I expected. She must feel my disappointment because she quickly continues. She will go back and check on the other three oocytes again later today to see if they also matured. If they have, they will be fertilised, too. She also let us know that our embryo transfer (ET) is scheduled for Monday, four days from now, at 7.30 in the morning. She kindly wishes us a great weekend and we hang up the phone.
I am sitting on the couch, trying to recall every single word of the conversation. My summary is this: yesterday we had five oocytes collected, two of them were definitely matured, but only one of the two was fertilised. However, there is still a possibility that we might have more fertilised oocytes by Monday. All of these facts play an equally important role.
I don’t allow myself too much time for an emotional breakdown. My analytical mind needs to inspect every fact that I have learnt today. It is time to turn to my best friend: Google. Here is what I learnt and why I call this the Numbers Game:
- There is a set number of follicles before the OCR. In our case this number was five follicles. BUT
- Some oocytes may be partially or completely damaged. I do not have any information on whether this has happened to our oocytes, so let’s just say that the number stays at five oocytes.
- There is a possibility that some of the follicles were empty, meaning, they did not contain any oocytes. In my case, each of my follicles had an oocyte inside of it, so our number is still five. BUT
- There is a chance that some of the collected oocytes were immature at the time of the OCR. Furthermore, some of them could be overly mature, as well. In our case the embryologist found two mature oocytes after the OCR but she will wait and see if the others will mature by the time of our embryo transfer. BUT…
When things finally start happening, you realise that the whole process is a true miracle.
Once your wife receives her hormonal stimulation, ideally more than 8 follicles begin to develop in her ovaries instead of just one. The hormone therapy is meant to increase the production of oocytes, however, your wife still needs her regular checkups during this process. The doctor will see what is happening inside of her ovaries using a simple ultrasound scan after five days of beginning hormonal stimulation. The most important question is how many healthy follicles will develop with the help of the stimulation.

One aspect I was curious about were the parameters of that particular sample compared to the previous one. Was this one better, worse or the same?
The number of follicles is important, but their size matters as well. The approximate diameter of a mature follicle is 18 millimetres, which actually surprised me at first - it is almost 2 centimetres! The oocyte that develops inside of the follicle is 0.1 to 0.2 mm, much smaller than the actual follicle. However, it is still large compared to a single sperm, which is approximately 45 micrometres from head to tail.
After the ovarian stimulation, my wife received another hormone therapy (called the “trigger shot”), which contains a human chorionic gonadotropin (hCG) to help the oocytes mature. Approximately 36 hours later our big day arrived: it was time for the oocyte retrieval and semen collection.
Oocyte retrieval is considered a minor surgery, but I was still a little bit concerned about it. I tried not to show it, of course, but I was worried about my wife. The procedure should take about 20 minutes, but it is still a surgery. Most of the time it is performed under general anaesthesia, especially if the woman has a greater number of available follicles. We only had five follicles after the ovarian stimulation, which is not ideal, but we were grateful to have at least some that were ready for the next step.
My wife was not under anaesthesia during the procedure, but the nurse gave her painkillers beforehand. According to her, she only felt some level of discomfort when the oocytes were suctioned out of her ovaries with a needle that went through her vaginal wall.
To clarify, during the oocyte retrieval process the doctor inserts a needle into each follicle and draws out all the fluid, including the matured oocytes. After just 10 minutes, she was done with this part.
During that same time, I came into the picture as well, or more precisely, my semen. The semen collection happens simultaneously with oocyte retrieval. By now I am used to not being the one at the centre of attention; most of the time I play the role of a supporting husband, but now it was my time to participate. Since I know my way around the clinic, I grabbed my cup and went to the collection room.
When the door closed behind me, I was left alone with thoughts and some porn magazines. Anyone who has ever been through this knows how awkward and uncomfortable this experience can be, but the staff at the clinic see many patients every day, so there is no need to feel embarrassed. Semen collection is an essential part of the IVF process, and it is just something that has to be done.
An unusual story to reassure you that there is no need to fear the oocyte retrieval procedure.
We woke up very early on the day of the oocyte retrieval (OCR). We had to be at the clinic by 7.30AM, as my OCR was scheduled for 9.30AM.
I followed the list of instructions I received by the clinic: slippers, robe, and ID cards ready to go. The only thing left to do was to iron my favourite nightie. My husband did it for me because first of all, he is much better at ironing than I am, and second of all, as he said, it was his participation in the oocyte retrieval. I was not allowed to eat, drink, or smoke after midnight, because the oocyte retrieval might be performed under general anaesthesia. The clinic also asked me to remove nail polish or artificial nails (but I don’t wear any so I did not have to concern myself with that).

I could not believe that altogether the whole procedure took only 10 minutes. I would not call it the most comfortable experience of my life, but I would definitely not call it painful either; if anything, it was absolutely tolerable.
We arrived at the clinic on time and as planned. After a quick check-in, during which we filled out several forms, we were asked to say goodbye for a while because we both had important tasks to fulfill separately. We had enough time for one more kiss and a “it’s going to be alright” hug - reassuring each other that everything will go smoothly.
A very kind nurse guided me to one of the preparation rooms and asked me to change and get ready for the procedure. When I stepped out of the bathroom in my freshly ironed nightie, I met a doctor in the room who wanted to have a last consultation with me before the oocyte collection. He informed me that due to the COVID-19 situation the hospitals are ordered to minimise the number of anaesthesia procedures (probably because the anaesthesiologists were busy with seriously ill Covid patients). He proceeded to explain to me that general anaesthesia is not absolutely necessary in my case because of my low egg count. He reassured me that all will be fine and promised me that there is nothing to worry about. I was not able to answer anything other than a very weak “OK”.
I asked for just five minutes to calm myself down a little bit. I laid down on the bed and tried my best to meditate (thank God I could finally use what I learnt in my online meditation classes). After a little while I got to take anti-anxiety medication prior to surgery. I would have preferred to take a few more than just one but the kind nurse reassures me that one would be enough.
While waiting for my painkiller injection, I started to recall everything that I have learnt about the oocyte collection procedure. The doctor will use an ultrasound probe with a needle attached to it, and he will insert the needle through the vaginal wall into my ovaries in order to reach my follicles. Afterwards, they are going to use the needle to suction out the fluid from the follicles and, hopefully, the oocyte will be retrieved along with it.
I have decided not to call my husband and tell him that I will undergo this procedure without general anaesthesia as I did not want to worry him during his semen collection. So I just continued to relax and meditate until it was time for the oocyte retrieval.
The nurse returned to let me know what the team was ready for me and she showed me the way to the surgery room. It looked similar to a normal gynaecology room except that everything looked and smelled very sterile. I was asked to lay down on the bed and they double checked my name and my birth date to make sure that all my oocytes were going to be labelled correctly. My doctor promised to explain everything to me throughout the procedure. He even showed me the monitor where, like he said, I could check if he was doing his job properly. On the screen I saw my five amazing follicles - they looked like little berries inside of a balloon.
The doctor then asked for my final confirmation to make sure that I was ready and he began the collection. I could only feel a slight sting during the insertion and right after that I could see how he reached the follicles one by one. After just a few minutes he told me that I did a great job and that we were DONE. My five incredible eggs came out of their follicles and they were ready to go to the lab to meet the “boys”. Mission accomplished!
I could not believe that altogether the whole procedure took only 10 minutes. I would not call it the most comfortable experience of my life, but I would definitely not call it painful either; if anything, it was absolutely tolerable. The main trick is to remain still and not move despite the discomfort.
I know that my story is a little bit unusual because 95% of you are going to have an oocyte retrieval under general anaesthesia, which will allow your surgeon to take their time to collect all of your oocytes - and hopefully it will be a greater number than in my case. Nevertheless, I felt like it was important to share my experience to reassure you that there is nothing to be afraid of during an oocyte retrieval.
Semen quality is not about masculinity. Unfortunately, a lot of men struggle with low semen quality these days. So, what can we do to help improve semen quality naturally?

In addition to vitamins and minerals, there are many other substances that have fertility promoting effects. Some of them include fenugreek seeds; tribulus terrestris, which increases semen viability; astaxanthin; Indian ginseng, also known as Ashwagandh;, aloe vera; royal jelly; cinnamon; green tea; red wine; brown beer; or dark chocolate. I am testing the last three, however, strictly in the recommended quantities. I strongly believe in them!
When it comes to male fertility, we talk about a lot of things that we need to give up, such as cigarettes, alcohol, or caffeine, and that we need to develop a healthy relationship with physical activity. We also have to consider lifestyle changes that are not easy to make for everyone. But what about changing our diet and choosing the right foods? We can find plenty of articles about nutrition and how it affects male fertility. It is easy to get lost in the abundance of information, and find out which suggestions have scientific proof to support it.
Simply put, sperm develops and matures within three months. With certain lifestyle changes, we can often achieve improvements to semen quality. However, it must be emphasized that these changes can improve semen quality, but that does not guarantee that a couple's fertility will increase, too. There are many parameters evaluated in the spermiogram, among others: the sperm count, the sperm shape, and the sperm motility. Another essential factor for healthy sperm is the energy to achieve their goal.
The good news is that there are plenty of simple things we can do to help improve our fertility health. So what can we do?
Drink plenty of plain water every day - at least 2 liters. I filled up a one-liter bottle with water and kept it with me at all times. I drank the first bottle before 11am, the second bottle by 3pm, and the last one before 7pm. It was a struggle in the beginning, but I got used to it in just one week and was able to keep up my good habit.
To positively influence semen quality, I also started making changes to my diet. The only recommendation that can currently be made to the general male population is to adhere to a healthy dietary pattern rich in plant-based foods such as in a Mediterranean diet; to reduce dairy consumption; and to give up processed foods (including salami and sausages, which I love). However, the good news is that one can eat a lot of seafood and fish due to their high content of omega-3 fatty acids.
A balanced diet is one of the most important factors for a healthy lifestyle. Extreme diets should be avoided; both low carb and high protein diets can hurt the semen quality - right now is not the time to go to any extremes!
Research has shown that free radicals may cause a decrease in semen quality, so the consumption of antioxidants, such as vitamin C, vitamin E, selenium, coenzyme Q-10, or L-carnitine, may help as well. The optimal intake of the following vitamins and minerals is the key to semen quality improvement:
- Zinc: the “fertility mineral”. It is one of the cornerstones of male fertility because it raises semen concentration, motility and testosterone levels. Natural sources include seafood, beef, lamb, chicken, nuts, legumes
- Selenium: an antioxidant that can improve semen concentration and motility. Natural sources include meat, sea fish, spinach, cabbage, mushrooms, beans, tomatoes, whole grains.
- Omega-3: essential fatty acids. They help with semen concentration, count, motility and improve its morphology. Natural Source include fish, shellfish.
- Vitamin C: an antioxidant. It improves almost all semen parameters. Natural sources include cabbage, broccoli, Brussels sprouts, cauliflower, parsley, paprika, radish, spinach, papaya, citrus fruits, strawberries, kiwi, black currant.
- B-9: Folate, the natural form of B9, also called folic acid in a synthetic form, promotes semen production, and is essential for DNA synthesis. Natural sources include legumes, eggs, nuts, green leafy vegetables, and ginger.
- B-12: Natural sources include beef, chicken, liver, salmon, tuna, eggs, seeds, cracklings, bananas.
- Vitamin E: an antioxidant. Natural sources include almonds, pumpkin seeds, sunflower seeds, sesame seeds, green leafy vegetables, vegetable oils, and avocado.
- Calcium: Natural sources include salmon, chia seeds, sardines, almonds, dark leafy vegetables, dried figs, oatmeal.
We can choose between natural sources that contain these minerals and vitamins but where exact quantities are unknown. Or we can opt for vitamin and mineral supplements that we can regularly consume in individual recommended quantities. Whichever route you choose, it's always a good idea to consult with your physician or fertility specialist to decide upon the right kinds and amounts. To make my (and my wife’s) life easier, I made a list of cooking ingredients to boost fertility and I tried to integrate as many of them into my daily diet as possible.
Why we need a Trigger Injection for oocyte maturation, and why it is so important to use it properly.
Let's learn the basics about the Trigger shot stage of the IVF treatment. Ovarian follicles are small fluid-filled sacs in the ovaries. Inside of each follicle is an immature egg, which grows and undergoes a set of changes. After the follicle reaches its optimal size, ovulation occurs and the mature egg is released.

After the Trigger Shot, I spent the next 36 hours before the egg retrieval relaxing and preparing myself for the egg collection.
During my ovarian stimulation period, I had two ultrasound appointments to check how my ovaries reacted to the hormone injections. I was quite surprised that a simple ultrasound test was able to detect my follicles. At the first appointment, we found four follicles, two on each ovary, and later on, one more little miracle follicle showed up on the screen. By the end of the stimulation stage, my ovaries developed five good looking follicles.
Five follicles is not a big number if we compare it to the optimal figure. Usually, anywhere between 8 and 15 follicles is considered an acceptable amount for an IVF treatment. Even though I received a fairly high dosage of fertility drugs, my ovaries reacted poorly to the stimulation. However, it only takes one egg to succeed, so the game has not been over yet!
The great news was that all of my follicles were a good size. When a follicle reaches the measurements between 16mm and 22mm, it is more likely that it contains a fully mature egg, which is ideal for the IVF process. All of my follicles reached this size, so it was definitely a small victory. The doctor also checked the thickness of my uterine lining, which was 12mm, and found it to be optimal for implantation.
The doctor gave us the green light to move forward to stage 2: the Trigger Shot, also called the Trigger Injection. The Trigger shot sends the eggs into meiosis (a state of reproductive division), and helps them to mature for egg collection. The objective is to decrease the number of chromosomes in the eggs from 46 to 23 prior to egg retrieval. If exactly 23 chromosomes are not present in the egg that undergoes fertilisation, it will not be able to create an embryo. I see now why it is so important.
The Trigger Shot usually contains the HCG hormone, which is the famous “pregnancy hormone” that we are looking for while taking a pregnancy test. After receiving the injection, ovulation can start between 36-48 hours. I had to use this single shot exactly 36 hours prior to my scheduled egg collection appointment. The most important step of the Trigger Shot is the timing; the success of the fertility treatment greatly depends on it and its effect on the quality of eggs. To make sure I did not forget this important task, I scheduled the shot in the Leeaf calendar, and waited for the selected time.
Injecting the Trigger Shot is exactly the same process as administering the daily hormonal stimulation shots, so there is nothing to be concerned about.
Even though we were rationally and emotionally prepared for hormonal stimulation, we were both stunned by some of the side effects.
Most couples who go through IVF for the first time, like us, are quite inexperienced and not very informed. Obviously, we asked a lot of questions and read as much information as possible about what to expect, however, actually experiencing this process first hand is fairly different. There are things that you just cannot fully prepare for. One of them is the amount of hormones your partner is going to receive and how she will react to it.

The main problem with hormonal stimulation is that the side effects are unpredictable. It affects everyone differently. Unfortunately, this part of the process cannot be avoided but you can get through it with a great deal of care.
The main question that came to me was: why does she need this huge amount of hormones? Well, hormones are used for many different things during the IVF treatment. Initially, the ovaries must be stimulated to grow as many follicles as possible. Then, the hormones help with maturation of the eggs before the actual egg retrieval. Also, certain hormones are used to improve the chances of embryo implantation. IVF is a precise process that requires exact doses of different hormones for each step, and that is why the final amount of hormones seems so excessive.
As it turned out, the stimulation process can be a little scary. My wife had to administer the hormone injections by herself. Do you understand? She has to poke herself with a needle every day for weeks. I still shudder as I write. And that is not all. Hormones can have two very perceptible side effects. One of them is that they can make your partner experience certain physical changes, the other can cause emotional tsunamis. Which one is worse? It is usually a tie, but both are definitely difficult issues.
I don’t know if we were lucky or we handled the situation well, but we only experienced one emotional side effect: my Love was able to laugh through her tears at practically anything, even in a completely neutral situation. The seven-headed dragon that I’ve read so much about was, fortunately, asleep.
On the contrary, dealing with the physical side effects was very difficult for her. Even though I tried to comfort her and reassure her that she is beautiful (which she truly is), it was hard for her to handle that her waist suddenly vanished and her belly doubled from bloating. Unfortunately, neither diet nor exercise helped, but after a few weeks it disappeared as it came. This is something that both of you should keep in mind.
Looking back, we can laugh at our experience now, but sadly, many women can have serious hormonal imbalances affecting them both physically and emotionally. This is one of the main reasons why many couples give up on IVF altogether, and that is completely understandable. Emotional support helps you both to be there for each other, to relieve the heavy pressure, which normally affects your partner more, and to handle the physical changes with ease.
A few tips to win over your fear of needles, and be a superwoman.
These days are about growing as many healthy, and mature eggs as possible with the help of ovarian stimulation. More eggs mean a better chance of succeeding.
According to my stimulation protocol I uploaded my medication plan to Leeaf, and also scheduled my next ultrasound appointment. This little extra help ensures me that all are on track. Being organized always comforts me.

That’s how I won over my fears of needles. I felt like an unstoppable superwoman every day after my injections, but to be honest, my fear was much bigger than realistic.
The day following my clinic visit, I had to administer my first daily hormone injection by myself. Of course – because of my nervousness – I was not sure anymore how to use the injection pen properly, even though the nurse gave me a proper training just 24 hours ago. The instruction book seemed a bit complicated to me, so I decided to go for an official Youtube tutorial. It’s better to check it twice, than doing anything wrong, right?
After double-checking the theory, I still had to deal with the reality: my fear of needles. This little problem won’t stop me for sure, but it makes me feel anxious. The needle is very tinny, but still - I am not professional – I am scarred that it’s going to hurt. I can be sure that 1 out of 4 women undergoing IVF has the same feeling as I do, because it's estimated that fear of needles affects up to 25% of adults. So, I am definitely not alone with this one either.
I did some research, and actually there are a few tricks we can do to make the daily injections easier:
- Ice the area before injecting so you can numb it.
- Pinch the skin at the injection site. Injections go right under the skin before you reach the muscle.
- Keep the muscle flaccid by standing on the leg opposite to the one in which you are injecting.
- Make sure to relax. Practice some deep breaths and make sure the muscle you are going to inject is loose.
- Pretend you’re braver than you feel. Count to three and shoot.
The system of fertility programs, based on my own experience, takes men as side characters. No problem at all, bad systems are there to break them
Did you know what ‘infertility’ means? The definition is very simple: if a couple has unprotected sex for 12 months and they are not able to conceive, they are labelled as infertile. I was sincerely surprised by this simple definition.
Unfortunately, most people still identify infertility as a ‘woman problem’. Although if we check on the main causes of infertility, we can find it easily that nothing can be further from the truth. For me, the turning point definitely was, when it turned out that - based on my spermiogram - I was an active participant in our lack of success. Before that I supported actively my wife, but then it became a completely different story. Even though if you have award-winning sperm quality, you still need to participate in the program with the same dedication as if it were all up to you.

"Don’t wait to be asked for staring in the movie. This is not Hollywood. It’s simply one, if not the most important movie of your life."
When I found myself in the world of IVF, I had to face the fact that everything is apparently all about the woman. In this story I felt like a “supporting family member”. There are a lot more tests and examination on her, some of them can be painful (fallopian test), and she even has to undergo a surgery (egg retrieval). These are the physical parts of the fertility program. I can’t take the hormones, or go under a surgery instead of her, even though I would do it happily. But there are many situations where I can make my partner’s job easier with my presence and support.
I don’t want to be a passive character in the story. I would like to have a child with her, such as much as she wants it. I can never leave her alone under any circumstances. I always want to be there for her, and make her feel, she can count on me. It’s also true if I play a more active role, I can own the process much more as well. It already makes an enormous difference when instead of saying ‘we have to undergo fertility treatment because my wife cannot have a child naturally’, I take it as ‘we, as a couple’ have fertility problems.
Your partner will need a constant emotional support. She is going to go through so many challenges over the process. Don’t be surprised if she laughs when she supposed to feel sad, and the other way around, and it won’t be the weirdest situation believe me. During these difficult weeks, you will be her rock, because you have to be.
The system of fertility programs, based on my own experience, takes men as side characters. No problem at all, bad systems are there to break them, it doesn’t have to be, work this way. Feel free to be more active in the process, first of all it will make your partner happy, and secondly you will be proud of yourself. Believe me, this will be very much needed too.
The first stage of our IVF cycle began with ovarian stimulation.
Per my doctor’s request, I went to the fertility clinic on the second day of my period for a final check up to make sure that it is safe to start our IVF treatment. The examination was quick and easy; it was only a simple ultrasound test and also the last pre-treatment evaluation, which is done to check the presence of any ovarian cysts. The absence of ovarian cysts is important because they can interfere with proper egg development during the treatment. Fortunately, there were no signs of any cysts, so nothing could hold us back from starting our fertility treatment this month. We were ready for stage 1: the ovarian stimulation.

I had to administer the hormone injections every day for five days. After that I came back to the clinic to find out how my ovaries reacted to the stimulation and how many follicles started to grow.
After the ultrasound examination, I received the stimulation protocol from my doctor. He explained that the medication plan is based on my previous test results. It is one of the reasons why we needed to do the previous blood tests. My AMH (anti-müllerian hormone) level was pretty low, so I needed a higher dosage of stimulation drugs.
But what actually is a controlled ovarian stimulation (COS)? During the ovarian stimulation phase of IVF, I used injectable fertility medication to stimulate my ovaries to produce multiple mature eggs. The injections that I used contained follicle stimulating hormone (FSH), which is necessary for ovaries to produce follicles, and luteinizing hormone (LH), which stimulates the growth of small follicles. The average length of the stimulation is 7-10 days, but in some cases it can take a couple of weeks before the medication starts working. The duration mainly depends on how the ovaries respond to the stimulation.
The right stimulation protocol highly affects the outcome of the treatment. I am sure that the process is more complicated than this, but generally speaking, if the stimulation dose is too small, none or only a small number of eggs are retrieved, and the IVF success rates decrease. On the other hand, if the dose of gonadotropins is too high, the woman is at a higher risk of hyperstimulation, also known as Ovarian Hyperstimulation Syndrome (OHSS). It is an exaggerated response to too many hormones and it can cause swelling to the ovaries, which can become painful. What is interesting about the whole stimulation process is that the same IVF protocol may work more successfully than others simply due to the different amount of available follicles. The instructions were clearly written down on the paper I received from the doctor, nevertheless, it was definitely comforting that a nurse explained everything about the injection pens and how to use them. I had to administer the first dosage of hormones to myself with the guidance of the nurse, and she said that I did it very well 🙂 Here are some tips from the nurse:
- Keep the drugs and the injectable pens in the fridge but leave them out at a room temperature for 20 minutes before administering them. Injecting a cold fluid can be unpleasant.
- Try to administer the injections in the same 4 hour window every day.
- To avoid skin irritation and soreness, alternate injection sites every day. One day use the right side of the belly (or the right thigh), the next day use the left side of the belly (or the left thigh).